Obesity is the root cause of several diseases, yet medical schools don’t train doctors on nutrition and weight loss.
Doctors are especially skilled for prescribing medications and performing surgery, but not for nutrition and weight loss.
You might be a little surprised to read that, but whether a physician has expertise regarding diet often comes down to their training and what they view as their circle of competence.
Medical training extends more than a decade, and yet there is barely any attention paid to nutrition or the equally thorny question of how a person should approach weight loss. In medical school, a standard curricula may include a mandated number of hours for nutrition, which can vary greatly depending on where a physician is trained. Generally speaking, during the four years of medical school, the total amount of time spent on nutrition is about 10 to 20 hours.
Medical school consist of nutrition lectures where is discussed things like the how vitamin D is activated in the kidney and skin. Yes, you might consider these subjects nutrition, but they are really much closer to biochemistry. So, not very useful knowledge when you’re trying to understand how to help people lose weight.
What people really want to know are things like, should I eat more carbs? Less carbs? More fat? Less fat? Is sugar bad? How do I lose weight? Those important health questions are apparently not considered the purview of many medical school teachings.

Medical school provide less training in real-life nutritional questions than most health clubs or gyms. As a result, doctors can be trained to believe that nutrition and weight loss are simply not part of the problems they deal with or should care about. Medical students model their self-image as a doctor on the mentors they meet in medical school. And those doctors and researchers often don’t prioritize nutrition or weight loss.
This contrasts starkly with the medical knowledge doctors do learn about. Everybody, and certainly every medical student, knows that obesity plays a dominant role in metabolic diseases like type 2 diabetes and metabolic syndrome. In turn, these metabolic diseases raise the risk of heart disease, stroke, cancer, kidney disease, blindness, amputations, and much more. Doctors understand the importance of weight gain in relation to disease, but not necessarily enough to educate themselves on how to lose weight or what people should or should not eat.
Given the knowledge that weight gain can lead to metabolic disease and other conditions like heart disease or diabetes, you’d assume a natural question from the medical community would be: What can I do to prevent or reverse weight gain (i.e., what’s the root cause)?
Instead, a doctor can be trained to think: weight gain can lead to metabolic disease and other problems like heart attacks. What drugs or surgery should I give to patients after they have their heart attack?
Obesity and metabolic disease are destroying our nation’s health, yet medical schools still do not adequately teach medical students or residents how to actually treat these problems. Doctors often tell patients to lose weight. What they don’t often tell patients, however, is how to lose it.
The entire medical school curriculum about weight loss largely comes down to the old advice: Eat less. Move more. Cut about 500 calories per day, and you will lose about a pound of fat per week.
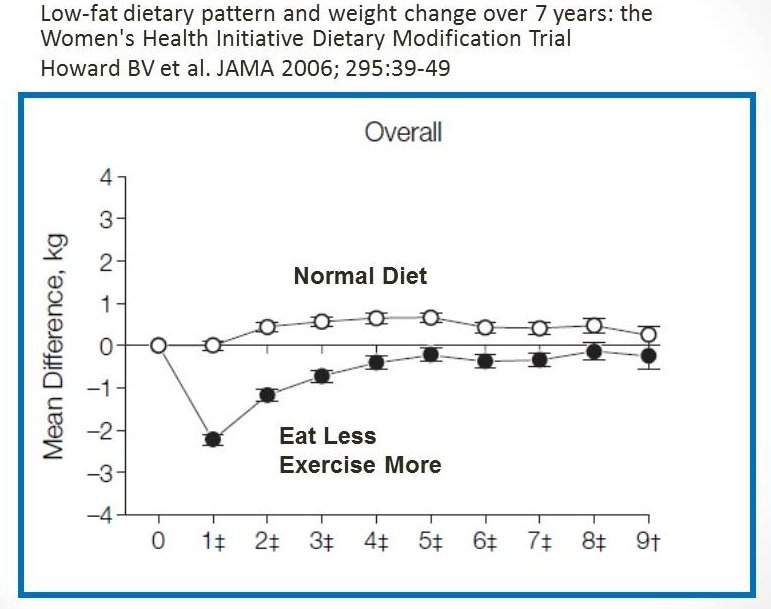
Doctors learn about this calorie-cutting method, but nobody seems to ask: Does it work? It doesn’t. People have tried this weight loss method for the last 50 years, and more often than not, it’s not effective over the long term. Most studies on calorie restriction for weight loss fail in one way or another. The success rate is about 1 percent. The most unfair part is that when patients return, unable to lose weight, they’re often blamed for their failure. It’s so much easier to blame the patient than to find fault in the standard medical advice of cutting calories.
Medical students are subjected to enormous unconscious bias. Doctors they know and learn from are not making nutrition a primary part of their practice. The understanding that nutrition is not something doctors do permeates. Doctors prescribe medications and perform surgery, but they don’t help with weight loss, even if it is the root cause of many of the diseases we see today. Thankfully there are other professionals who study nutrition, like registered dietitians, but it makes no sense that doctors do as little as possible to address this underlying health problem.
Does this change after medical school? Yes, it gets worse. Speciality training, internship, residency, and fellowship are another five years of training after medical school where there is typically no formal curriculum around nutrition. That’s another five years where doctors learn that weight loss has nothing to do with them.

Should you talk to your doctor about weight loss? Would you ask your plumber to remove your wisdom teeth? Would you ask your barista to check your vision?
If doctors truly want people to be well, they must start caring about nutrition and guiding people through weight loss. There’s no longer any excuse not to. They should include more nutrition in the curriculum of medical schools or residency training. They need to learn a bit more of the physiology behind weight loss and weight gain, the hormonal regulators of weight and how to influence them using diet.
The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health provider regarding any questions you may have about a medical condition or health objectives.





